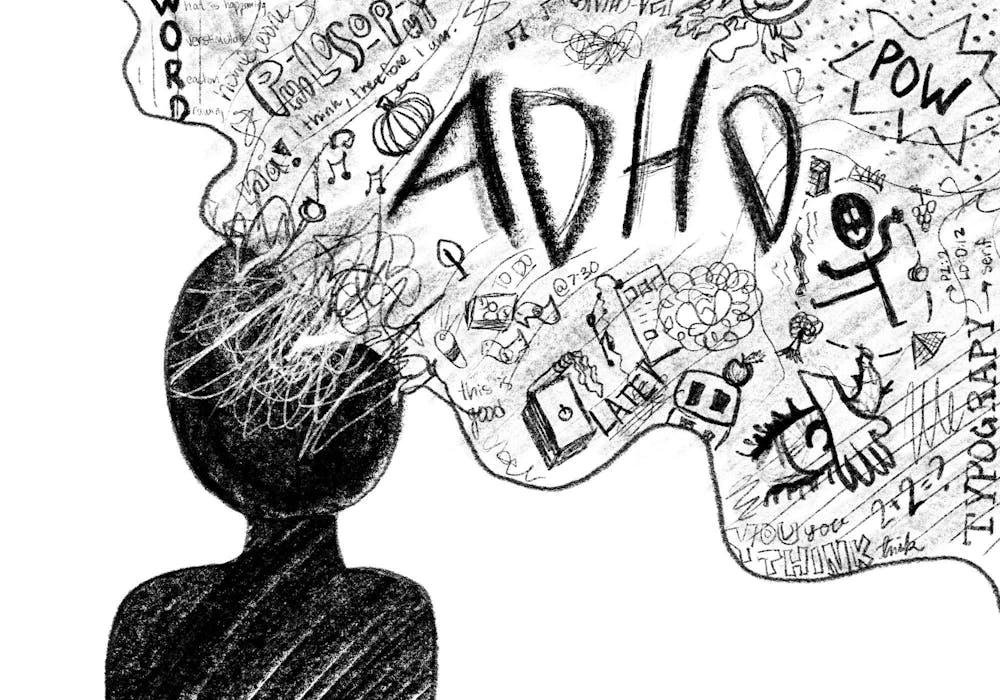
A neurodevelopmental disorder known as attention deficit hyperactivity disorder (ADHD) is typified by recurrent patterns of impulsivity, hyperactivity, and inattention. It impacts both adults and children, and its symptoms can have a major negative influence on day-to-day activities and overall well-being. Due to the intricacy of ADHD, there are many different treatment modalities available, with medication serving as a mainstay for many patients. This article delves into the most recent developments in ADHD medicine, with the goal of demystifying the therapies and offering a thorough rundown of fresh, practical choices.
Recognizing ADHD
Three main subtypes of ADHD exist: mixed presentation, hyperactive-impulsive, and mainly inattentive. Although the precise origin of ADHD is still unknown, a mix of neurological, environmental, and genetic variables are thought to be involved. Studies on brain imaging have revealed variations in the structure and activity of the brain in people with ADHD, especially in domains pertaining to impulse control, executive function, and attention.
Conventional ADHD Drugs
Stimulant drugs have been the first choice for treating ADHD for many years. These include amphetamine-based drugs (Vyvanse, Adderall) and methylphenidate (Ritalin, Concerta). Dopamine and norepinephrine, which are released in the brain in response to stimulants, are known to enhance attention and decrease impulsivity and hyperactivity. These drugs can have side effects like elevated heart rate, appetite suppression, and insomnia even though they work well.
Non-Stimulating Drugs
Although many people find stimulants useful, not everyone is a good fit for them. An option is provided by non-stimulant drugs, especially for those who are adversely affected by stimulants or do not respond well to them. One such drug is strattera, also known as atomoxetine. It is a selective norepinephrine reuptake inhibitor (NRI) that works by raising norepinephrine levels in the brain to help improve concentration and decrease impulsivity. Alpha-2 adrenergic agonists guanfacine (Intuniv) and clonidine (Kapvay) were first prescribed to treat excessive blood pressure but were later discovered to be useful in treating symptoms of ADHD, especially in lowering hyperactivity and enhancing executive function.
Developments in ADHD Drugs
Medication for ADHD has come a long way in recent years, with the main goals being increased treatment options, decreased side effects, and increased efficacy.
1. Prolonged-Release Mixtures
The creation of extended-release (ER) forms for already-approved drugs is one significant development. These formulations minimize drug level peaks and troughs that may cause side effects by delivering a consistent release of the medication throughout the day, eliminating the need for several doses. Adderall XR, Concerta, and Vyvanse are a few examples. Extended-release drug formulations offer more reliable symptom relief and increased adherence to prescription schedules.
2. New Sources of Stimulation
New drugs that contain stimulants and have special benefits have recently been approved as a result of advances. For instance, Jornay PM is a methylphenidate-based drug that is intended to be taken at night, with its effects starting to manifest the following morning. This tackles the problem of controlling morning symptoms, which can be especially challenging for kids getting ready for school. Other examples include Adzenys XR-ODT and Cotempla XR-ODT, which provide easier-to-administer oral disintegrating tablet formulations, especially for kids who have trouble swallowing pills.
3. Innovations Without Stimulants
Notable advancements have also been made with non-stimulant drugs. In 2021, the FDA approved a novel non-stimulant called viloxazine, sometimes known as Qelbree, to treat ADHD in children and adolescents. Like atomoxetine, it is a selective norepinephrine reuptake inhibitor, but because of its unique chemical makeup, it may have a different profile of side effects. According to clinical investigations, viloxazine can considerably lessen symptoms of ADHD while lowering the risk of side effects commonly associated with stimulants.
4. Individualized Medical Care
In the context of treating ADHD, the idea of individualized medicine is becoming more popular. Treatments are being customized to the patient's specific genetic profile through the use of pharmacogenetic testing, which examines how a person's genetic composition influences how they respond to drugs. Using genetic markers to determine the best drug, this method seeks to maximize effectiveness and reduce negative effects.
5. Digital Medicine
An interesting new area in the treatment of ADHD is represented by digital therapies. The first FDA-approved prescription video game created specifically to help kids with ADHD focus better is called EndeavorRx. Through gameplay, it addresses particular brain processes and provides a non-pharmacological option that can be used in addition to conventional drugs. Digital therapies offer a fresh method of treating ADHD symptoms, and kids and teenagers may find them very interesting.
Obstacles and Things to Think About
Even with these developments, treating ADHD is still difficult. Every person reacts to drugs differently, so it's frequently necessary to go through a trial-and-error process to determine the best course of action. Furthermore, there is worry about the possibility of stimulant medicine abuse and misuse, especially in young people and adolescents. Healthcare professionals need to weigh the advantages and disadvantages of prescription drugs while keeping a watchful eye out for any indications of abuse.
The adverse effects are still a major factor. Insomnia, decreased appetite, weight loss, elevated blood pressure, and possible cardiovascular problems are typical side effects of stimulant drugs. Even while they typically have less adverse effects, non-stimulant drugs can sometimes result in problems like gastrointestinal distress, mood fluctuations, and exhaustion. The long-term effects of ADHD drugs are not entirely understood, thus more research and observation are required.
Accessibility and cost are further obstacles to successful treatment. Insurance coverage varies and new drugs and formulations might be costly. One of the most important public health objectives is to guarantee that everyone with ADHD, regardless of socioeconomic background, has access to efficient treatments.
Prospective Courses
Treatment for ADHD appears to have a bright future because to ongoing research in several important areas:
1. Identification of Biomarkers
The treatment of ADHD may undergo a radical change if biomarkers that indicate a patient's reaction to a particular drug are found. Based on an individual's biological traits, biomarkers can assist clinicians choose the most effective drug for them. Biomarkers are quantifiable indications of a biological state or condition.
2. Neurofeedback
One kind of biofeedback called neurofeedback teaches brain self-regulation through real-time monitoring of brain activity. It has demonstrated potential in treating symptoms of ADHD by teaching people self-control over their attention and impulses. Neurofeedback is still regarded as experimental, although it has the potential to be an effective technique in the treatment of ADHD.
3. Combination Treatments
Another area of focus is the combination of behavioral therapy and medicines. Behavioral treatments that improve functioning and manage symptoms of ADHD include parent education programs and cognitive-behavioral therapy (CBT). Integrating them with pharmaceutical interventions could yield a more all-encompassing and efficient strategy.
4. Progress in Non-Pharmaceutical Interventions
The body of knowledge about non-pharmacological therapies, like diet, exercise, and mindfulness, is still expanding. These methods don't carry the same danger of adverse effects as conventional drugs and can provide further benefits. Research is still being done to see how these treatments can be used into a comprehensive treatment strategy.
In summary
Due to the intricate and varied nature of ADHD, treatment must be tailored to the patient. The field of ADHD drugs is always changing as a result of the development of fresh, efficient therapies that give people with ADHD hope for better symptom management and a higher quality of life. Improvements in ADHD therapy are opening the door to more efficient and customized care, from innovative stimulants and extended-release formulations to digital treatments and personalized medicine.
The objective is still to develop safe, efficient, and widely available therapies for ADHD in all people as research advances. A thorough grasp of each patient's particular demands combined with ongoing innovation will be crucial to reaching this objective. We can better assist and enable the flourishing of individuals with ADHD if we debunk the myths surrounding ADHD drugs and welcome innovative, efficacious therapies.